Dan O'Neill
@dp_oneill
Healthcare services, tech & policy nerd. Alum: @theNAMedicine, @StanfordEng, @SAISHopkins, @CMCnews, @BCG and various health services & tech cos. Views my own.
ID: 1494021152
https://dponeill.com/ 08-06-2013 21:59:21
7,7K Tweet
5,5K Takipçi
796 Takip Edilen






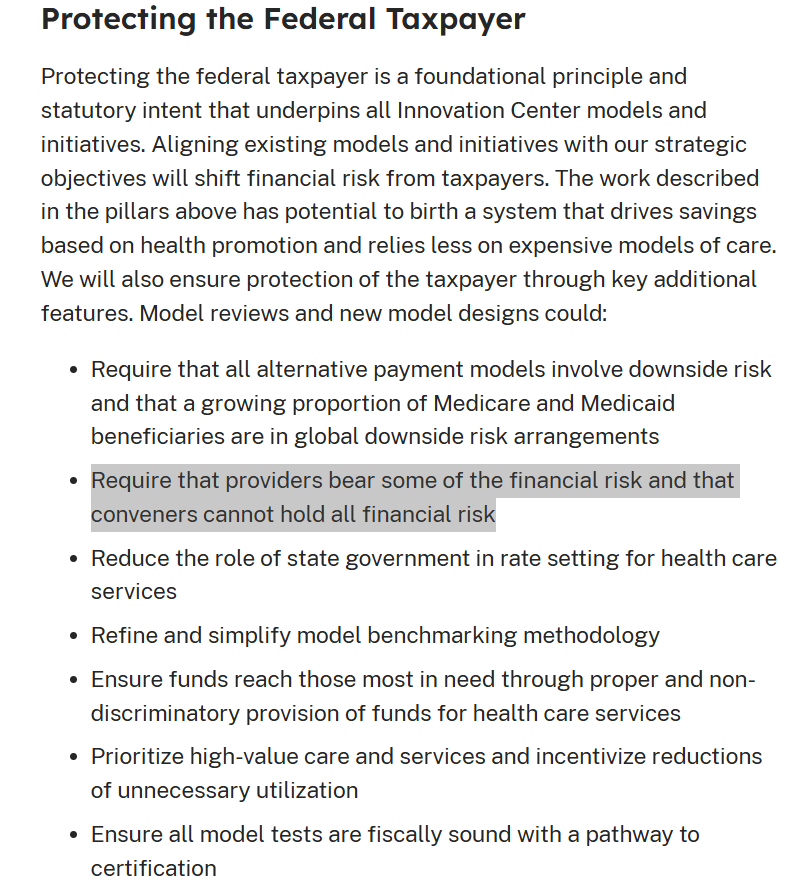
This is a healthy change from CMS Innovation Center. When conveners hold most or all financial risk, they unwind the incentives that CMS is trying to create. Same problem when MA plans do risk deals with IPAs, which then pay PCPs fee-for-service or a flat cap rate. Largely useless.





Interesting study, suggesting that employers in Colorado mountain towns lowered premiums by 13-17% by collectively negotiating lower provider prices. Perhaps a bit like Germany, which has private providers & plans but uniform regional fee schedules. onlinelibrary.wiley.com/doi/10.1111/jo…

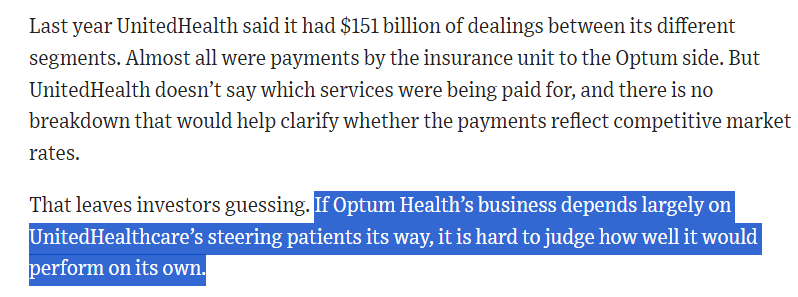
Pretty clear The Wall Street Journal summary of concerns about vertically-integrated insurers (not just UHC!). The "provider" subsidiaries do depend on the parent insurer steering patients their way. And, what's not mentioned - the insurer obligating independent providers to contract with that sub