Dr Dee Sanchez
@deeoptimal
MD, MIS, PMP, NREMT, NASM-CPT, FAWM Candidate | EM PGY1| IG= @drdee2022 |
Passions: #wildernessmed #medinformatics #ems #emergencymed #tweetsnotmedicaladvice
ID: 3045659019
https://instagram.com/drdee2022?utm_medium=copy_link 20-02-2015 04:26:46
1,1K Tweet
83 Followers
194 Following

To prevent thrombosis use the Tunneling Technique: catheter thru tunnel created by 13G angiogram off label. #resusfest TheVascularGuy


So excited for Haney Mallemat surprise live call into #resusfest!! He will be presenting on what to do after we got ROSC!


The period immediately following ROSC holds the highest potential for rearrest. Therefore, our main goal during this time is to stabilize the patient in order to avoid cardiac arrest. Haney Mallemat #resusfest


Mallemat recommends cycling the BP cuff every 1-2 minutes to monitor for hypotension (in the absence of an arterial line). Haney Mallemat #resusfest

Assess end-tidal CO2; when CO2 drops below 30 mmHg, there is an increased risk for rearrest. Use auditory feedback to your advantage by setting the pulse oximeter on the auditory setting and listening for tone and frequency changes. Haney Mallemat #resusfest


After ROSC, order: ➡️lactate levels ➡️arterial blood gas (ABG) with “shock panel” (which is also known as ABG+) ➡️tox panel. Look for acetaminophen and salicylates, esp if a cause or the arrest has not been determined ➡️ blood cultures Haney Mallemat #resusfest


After ROSC, ➡️Transition vasopressor to a formal drip ➡️Continue an antiarrhythmic infusion ➡️Consider analgesia and sedation Haney Mallemat #resusfest

Airway management after ROSC: ⭐️hemodynamics is more important; focus on airway mgt after hemodynamic stability has been achieved. ⭐️consider swapping out SGAs/EGAs to a formal ETT Haney Mallemat #resusfest

After ROSC has been achieved do a team debrief. It is crucial to take at least 5 mins to discuss with the entire team what went well, what can be done better, and address any lingering thoughts regarding the case. Haney Mallemat #resusfest


45min post-ROSC: ➡️focus on fine-tuning tx to max survival by fine-tuning airway management, access, and optimizing MAP (goal is 65). ➡️Adjust vent settings to a tidal volume consistent with PT ideal body weight. ➡️Use vasopressors to maintain MAP at goal. Haney Mallemat

In the event PT needs more time in ED after ROSC: ➡️preserve neuro fx; monitor EEG. ➡️ poor data to support empiric ABX, instead start steroids. ➡️Maint. fluids not needed & can cause harm due to excess fluid in the interstitium.Haney Mallemat





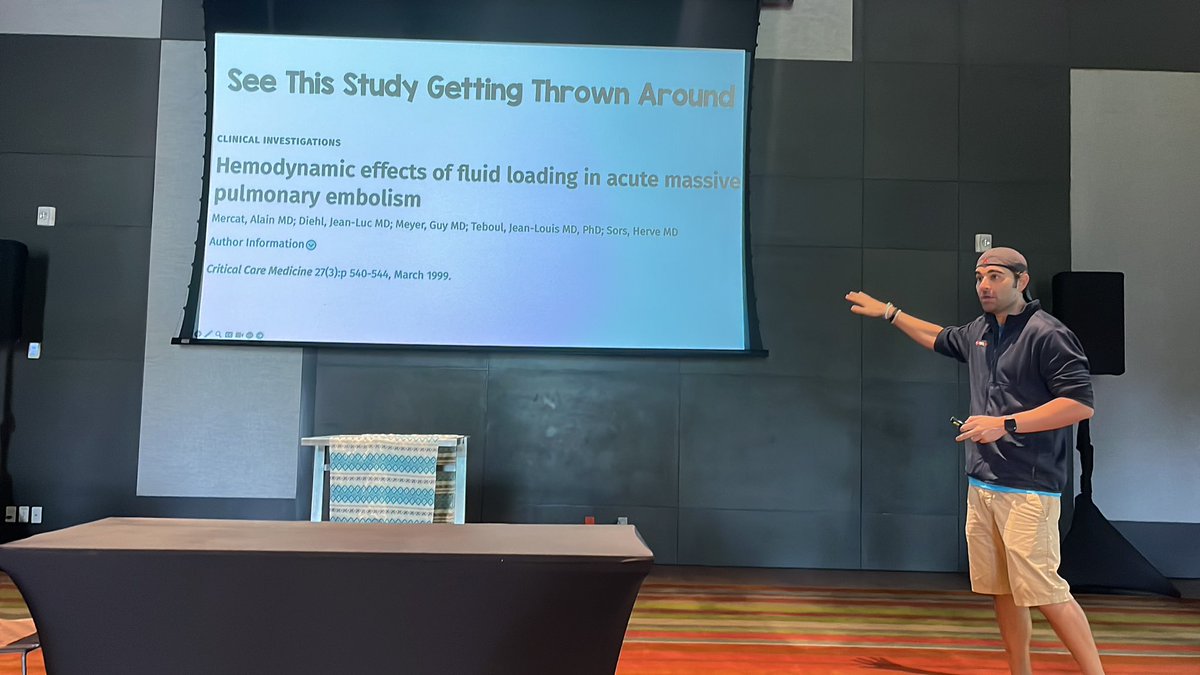
In massive pulmonary embolism, should we give fluids or not? Being covered today by Salim R. Rezaie, MD at #resusfest


PE is an afterload problem. Hypotension with tachy = cardiogenic shock due to RV strain/failure. Thus giving fluids won’t fix PE spiral of death. PPL who think fluids of 500ml for PE are WRONG. only study of support was in 1999 & not on for massive PE. Salim R. Rezaie, MD #resusfest

In PE how to alteplase: Salim R. Rezaie, MD plan of action is to give 10mg bolus then 40mg over 2 hours. The idea is to HALF-DOSE your thrombolysis. Thus if you are giving 100mg now then give half dose (ie. 50) Salim R. Rezaie, MD #resusfest